The Silent Vision Thief
Glaucoma is often referred to as the “silent thief of sight”. This is because it can gradually damage the optic nerve without noticeable symptoms until significant vision loss occurs. This group of eye diseases is one of the leading causes of irreversible blindness worldwide, making early detection and timely treatment essential. Damage associated with glaucoma is permanent. However, its progression can be stopped with proper care, preserving vision for as long as possible.
Types and Causes
Types
There are several types of glaucoma, but the two main forms include:
- Primary Open-Angle Glaucoma (POAG): This type of glaucoma is the most common., It occurs when the drainage angle formed by the cornea and iris remains open, but the trabecular meshwork becomes partially blocked over time, resulting in increased intraocular pressure (IOP) and gradual damage to the optic nerve.
- Angle-Closure Glaucoma (ACG): This type of glaucoma is rare. It occurs when the iris appears to be forward, narrowing or blocking the drainage angle, causing a sudden rise in eye pressure. This is a medical emergency requiring immediate care to prevent permanent vision loss.
Other types include Normal-Tension Glaucoma (NTG). Here, optic nerve damage takes place despite normal intraocular pressure. Further, Congenital Glaucoma, which is present at birth due to abnormal eye development.
Causes
The exact cause of glaucoma is not clear. However, it typically involves increased intraocular pressure due to improper drainage of aqueous humour, the clear fluid inside the eye. Over time, this pressure causes damage to the optic nerve, which is responsible for sending visual signals to the brain. Other contributing factors include poor blood flow to the optic nerve, genetic predisposition, and structural abnormalities in the eye.
Risk Factors
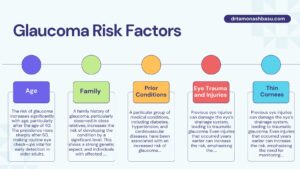
Age
The risk of glaucoma increases significantly with age, particularly after the age of 40. The prevalence rises sharply after 60, making routine eye check-ups vital for early detection in older adults.
Family
A family history of glaucoma, particularly observed in close relatives, increases the risk of developing the condition by a significant level. This shows a strong genetic aspect, and individuals with affected family members should undergo regular screenings.
Prior Conditions
A particular group of medical conditions, including diabetes, hypertension, and cardiovascular diseases, have been associated with an increased risk of glaucoma. In addition, individuals with high eye pressure (ocular hypertension) are at greater risk of progressing to glaucoma.
Eye Trauma and Injuries
Previous eye injuries can damage the eye’s drainage system, leading to traumatic glaucoma. Even injuries that occurred years earlier can increase the risk, emphasising the need for monitoring after eye trauma.
Thin Corneas
People with thin central corneal thickness are at higher risk for developing glaucoma, as thin corneas may lead to underestimation of intraocular pressure during routine eye checks, potentially delaying diagnosis.
Watch out For These Symptoms
Glaucoma often progresses silently, but some symptoms may signal its presence, particularly in acute forms like angle-closure glaucoma. These include:
- Blurred vision
- Seeing halos around lights
- Severe eye pain
- Headaches
- Nausea and vomiting
- Sudden loss of vision
In most cases of open-angle glaucoma, there are no early warning signs, and peripheral vision gradually diminishes over time. By the time central vision is affected, significant and irreversible damage may have already occurred, making regular eye exams essential, especially for those with risk factors.
Detection and Treatment
Early detection of glaucoma is very important for retaining vision. Comprehensive eye exams, including intraocular pressure measurement, optic nerve assessment, visual field testing, and imaging studies like Optical Coherence Tomography (OCT), help in diagnosing glaucoma early. Regular eye check-ups, particularly after age 40, or earlier for those with risk factors, can facilitate early intervention and slow disease progression.
Treatment Options
While glaucoma-related vision loss is irreversible, treatment can prevent further damage. Treatment options include:
Medications:
- Prescription eye drops are often the first line of treatment to decrease intraocular pressure, either by decreasing fluid production within the eye or improving its drainage.
Laser Therapy:
- Laser Trabeculoplasty (for open-angle glaucoma) helps improve fluid drainage.
- Laser Iridotomy (for angle-closure glaucoma) creates a small opening in the iris to improve fluid flow.
Surgical Procedures:
- Trabeculectomy: A surgical procedure that creates a new drainage pathway.
- Glaucoma Drainage Implants: Devices applied to help drain excess fluid.
- Minimally Invasive Glaucoma Surgery (MIGS): Less invasive options with quicker recovery and fewer complications.
Treatment plans are customised based on the type and severity of glaucoma, intraocular pressure levels, and individual patient factors.
Further Tips
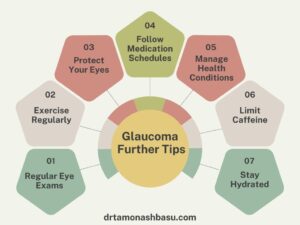
In addition to treatment, lifestyle adjustments can support eye health:
- Regular Eye Exams: Schedule routine check-ups, especially if you have risk factors.
- Exercise Regularly: Moderate exercise can help reduce eye pressure, but consult your doctor about safe activities.
- Protect Your Eyes: Use protective eyewear to minimise injuries during activities with a risk of eye trauma.
- Follow Medication Schedules: Uniformity in using prescribed eye drops is vital for controlling intraocular pressure.
- Manage Health Conditions: Manage diabetes and hypertension, as these conditions can contribute to glaucoma progression.
- Limit Caffeine: Excessive caffeine intake can increase eye pressure in some individuals.
- Stay Hydrated: Drink fluids in small amounts throughout the day to avoid sudden pressure spikes.
Schedule Your Appointment Today:
- Phone:8544042768
- Online Booking: click here
Conclusion
Glaucoma is one of the leading causes of permanent blindness globally, primarily because it often develops silently without early symptoms. Understanding the risk factors—age, family history, previous conditions, eye trauma, and thin corneas—and undergoing regular eye exams can aid in early detection and timely treatment.
While glaucoma cannot be cured, its progression can be slowed through medications, laser therapy, or surgery, preserving vision and improving quality of life. Awareness, proactive monitoring, and adherence to treatment plans are the keys to protecting your vision from this silent thief. If you fall within a high-risk category or notice any suspicious symptoms, consult your ophthalmologist promptly to safeguard your eye health.